Introduction: The lymphoma microenvironment is increasingly recognized as crucial to sustaining lymphoma cell growth and an important contributor to treatment outcome, especially in the context of immunotherapies. CD20-targeted monoclonal antibodies (e.g. obinutuzumab [G] and rituximab [R]) function by several mechanisms, including antibody-dependent cellular cytotoxicity/phagocytosis (ADCC/ADCP). Immune effector cells, such as natural killer (NK) cells and phagocytes (i.e. macrophages and dendritic cells), and the Fc gamma receptor (FcγR) found on the surface of these cells, are critical to antibody treatment efficacy. Here we evaluated how the lymphoma microenvironment may affect clinical outcome in patients (pts) with previously untreated diffuse large B-cell lymphoma (DLBCL) receiving immunochemotherapy.
Methods: We leveraged two large Phase III clinical trials of pts with previously untreated DLBCL (GOYA [NCT01287741] and MAIN [NCT00486759]) to produce comprehensive lymphoma immune microenvironment profiles from 604 tissue biopsies from pts treated with R plus cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) or G plus CHOP (G-CHOP) using the RNA-Seq deconvolution and marker gene methods: quanTIseq and xCell. The infiltration scores in each pt for various immune and stromal cell types were assessed, and their contribution to disease biology and treatment outcome was examined.
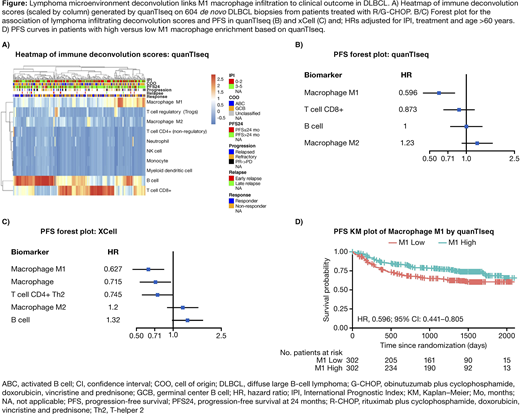
Results: The extent of lymphoma microenvironment heterogeneity highlighted by the deconvolution analyses was consistent with previous studies (Figure A). Of the infiltrating cell types analyzed, the M1 macrophage signature quantified by either quanTIseq or xCell was most strongly associated with lower risk of progression (progression-free survival [PFS]; quanTIseq: HR, 0.596; 95% CI: 0.441-0.805; 24-month PFS: 82% [M1 high] vs 68% [M1 low] and xCell: HR, 0.627; 95% CI: 0.465-0.844; 24-month PFS: 80% [M1 high] vs 70% [M1 Low]; Figure B, C, D) and improved overall survival (OS; quanTIseq: HR, 0.465; 95% CI: 0.318-0.679; and xCell: HR, 0.527; 95% CI: 0.365-0.762). This finding was confirmed by both algorithms. This prognostic trend was stronger amongst G-treated pts than R-treated pts, consistent with the previous finding that G exhibits higher ADCC versus R (Mössner, et al. Blood 2010). Pts with PFS >24 months had significantly higher levels of M1 macrophage scores than pts with PFS <24 months. Despite the correlation with delayed disease progression, there was no differential enrichment of M1 macrophages in pts with complete response versus non-responders at end of treatment, or depending on International Prognostic Index. M1 scores did not significantly differ depending on cell of origin, although there was a trend for higher M1 macrophage scores in germinal center B-cell DLBCL. Aside from M1 macrophages, CD4+Th2 cells showed the strongest prognostic trend in DLBCL (PFS; HR, 0.745; 95% CI: 0.553-1.000; Figure C). In contrast to M1 macrophages, pts with M2 macrophage infiltration tended to have shorter PFS and OS although relatively low levels were observed for these signatures (Figure B, C). This suggests that lymphoma-infiltrating macrophages more commonly resemble the classically activated M1 polarization phenotype and are linked to prolonged PFS, while alternatively activated M2 macrophages, although their frequency is lower in DLBCL, are associated with shorter PFS. Consistent with previous work showing that programmed death-ligand 1 (PD-L1) levels correlate with a macrophage signature in DLBCL (McCord, et al. Blood Adv 2019), M1, but not M2, macrophage infiltration correlated with PD-L1 mRNA expression. M1 enrichment was highly correlated with CD8+ T cell signatures (including central and effector memory CD8+ T cells) in DLBCL.
Conclusions: Data suggest macrophage polarization may be an important contributor to immunochemotherapy outcome in DLBCL. Previous studies aiming to link tumor-associated macrophages to R-CHOP outcome have yielded conflicting results, perhaps as most relied on CD68/CD163 staining alone as markers. Although R and G are thought to function via NK cell-mediated ADCC, FcγR-dependent stimulation of M1 macrophage-mediated ADCP may be key to sustaining their anti-lymphoma activity. Strategies facilitating the recruitment of M1 macrophages or macrophage repolarization may augment responses to immunochemotherapy in DLBCL.
Yan:F. Hoffmann-La Roche: Current Employment, Current equity holder in publicly-traded company. Chang:F. Hoffmann-La Roche: Current Employment, Current equity holder in private company. Raghavan:F. Hoffmann-La Roche: Current Employment. Dong:In graduate school: University of Toronto, MSc Biostatistics: Ended employment in the past 24 months; F. Hoffmann-La Roche, Mississauga, Biometrics: Current Employment. Klein:Roche: Current Employment, Current equity holder in publicly-traded company, Patents & Royalties. Nielsen:F. Hoffmann-La Roche: Current Employment, Current equity holder in publicly-traded company. Paulson:Genentech, Inc: Current Employment; F. Hoffmann-La Roche: Current equity holder in private company, Current equity holder in publicly-traded company. Hatzi:F. Hoffmann-La Roche: Current equity holder in publicly-traded company; Genentech, Inc.: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.